- New REMS for Immediate-Release Opioids in Outpatient Settings – Training for Pharmacists and Nurses, Not Just Prescribers (ptcommunity.com)
The FDA has approved a final Opioid Analgesic Risk Evaluation and Mitigation Strategy (REMS) that includes several measures to help better communicate the serious risks about the use of opioid pain medications to patients and health care professionals. This expanded REMS, for the first time...
- ….applies to immediate-release (IR) opioid analgesics intended for use in an outpatient setting. The new REMS also applies to the extended-release and long-acting (ER/LA) opioid analgesics…
- ….training be made available to health care providers who are involved in the management of patients with pain (e.g., nurses and pharmacists), and not only to prescribers.
- ...education cover broader information about appropriate pain management, including alternatives to opioids for the treatment of pain.
- ...new product labeling containing information about the health care provider education available through the new REMS.
- ,,,the agency has approved the new FDA Opioid Analgesic REMS Education Blueprint for Health Care Providers Involved in the Treatment and Monitoring of Patients with Pain (Blueprint). This includes updated educational content.
- Nevada Medicaid approves policy requiring prior approval after 5 therapy sessions (thenevadaindependent.com)
Nevada Medicaid approved a requirement that therapists receive prior approval before providing more than five therapy sessions to a patient...The new policy, which takes effect on Oct. 1, will require psychologists, therapists and other mental health providers to submit written documentation to the state’s third-party vendor demonstrating the medical necessity of treatment and receive prior approval to continue providing both talk therapy and neurotherapy services after five sessions with a patient. The final policy is a scaled back version of earlier proposals from Medicaid to require prior authorization before the first session or after three sessions, both which received significant pushback from the mental health community over the last few weeks...The policy will only apply to patients enrolled in Medicaid’s fee-for-service program, in which Nevada Medicaid reimburses individual providers for services rendered, and not those who are covered under Medicaid managed care, where the state pays an insurance company a flat fee to provide health services to a patient. About one in four of the 650,000 Nevadans on Medicaid are enrolled in the fee-for-service-program.
- Experts weigh in on CMS’ big changes to clinical documentation, EHRs and interoperability (healthcareitnews.com)
Industry groups like easier quality reporting and advance applications of telehealth, but some say docs shouldn't have to make expensive EHR upgrades for 2019..."historic changes" announced...by the Centers for Medicare & Medicaid Services, promising big adjustments to its policies around the Physician Fee Schedule and the Quality Payment Program, already have the healthcare industry talking...CMS says it wants to incentivize the use of and access to virtual care and telehealth, to ease the quality reporting burden on physicians by focusing on the most important and impactful measures...also wants to spur better information sharing among healthcare providers, regardless of what electronic health record vendor they happen to use...CMS notes that these proposals will modernize Medicare payment policies to promote access to virtual care, saving Medicare beneficiaries time and money while improving their access to high-quality services no matter where they live...the new proposal would "help shift the nation’s electronic documentation away from overly long, form-driven, hard-to-read documents written primarily to satisfy billing requirements to what it was originally intended for – providing high- quality care to patients."...
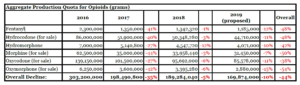
- Trump administration proposes production quota cuts for six opioids (reuters.com)Proposed Aggregate Production Quotas for Schedule I and II Controlled Substances and Assessment of Annual Needs for the List I Chemicals Ephedrine, Pseudoephedrine, and Phenylpropanolamine for 2019 (justice.gov)
The Trump administration on Thursday proposed that U.S. drugmakers cut production quotas of the six most abused opioids by 10 percent next year to fight a nationwide addiction crisis....the U.S. Justice Department and Drug Enforcement Administration said the proposed cut would be in keeping with President Donald Trump’s effort to cut opioid prescription fills by one-third within three years...
- Mental health providers concerned about proposed limits on therapy sessions for Medicaid patients without prior approval (thenevadaindependent.com)Nevada Medicaid shift could impact continuity of mental health care (reviewjournal.com)
Nevada Medicaid will decide next month whether to impose additional requirements for patients to undergo therapy on an ongoing basis, a move the state says will increase accountability and ensure people are getting the care they actually need...mental health providers across the state are decrying as yet another barrier to access to mental health care for a vulnerable population...The Division of Health Care Financing and Policy...to decide whether to require psychologists, therapists and other mental health professionals to provide written documentation demonstrating medical necessity and receive prior approval to continue providing talk therapy or neurotherapy…State officials describe the policy as an effort to be both fiscally and socially responsible, ensuring that providers are only getting paid for services that are actually necessary and that patients are receiving the right treatment for their condition...opponents...argue that it will damage an already-thin safety net for patients by imposing additional administrative burdens on providers…
- Pfizer Caving to Trump Has Wall Street Asking Who’s Next (bloomberg.com)Sen. Wyden probes 'secret, sweetheart' deal between Pfizer, Trump (fiercepharma.com)
Pfizer’s decision to delay planned drug price hikes after President Trump attacked the company on Twitter may cause another shakeout throughout the health-care industry. Analysts at Goldman Sachs, Morgan Stanley and SunTrust expect other drugmakers will have to show more restraint on price increases, and say drug distributors may also find themselves under pressure. Height Capital Markets earlier cautioned about the risk to pharmacy-benefit managers, saying that Pfizer’s move ups the ante for the White House to propose policy changes on the use of rebates...“Drug stocks will not react favorably to this news, given the chilling effect this will likely have on others looking to take price increases. On the one hand, the price increases taken in July are only a small number of increases taken over the past year or several years, so the impact of the rollback to the healthcare system is insignificant in the big picture. However, the impact on the broader [dialogue] is much larger.”
- Moody’s: CMS proposed changes to Medicare’s outpatient prospective payment system could hurt hospitals (healthcarefinancenews.com)
...the Centers for Medicare and Medicaid Services' proposed changes to outpatient services, including site neutral clinic visits, 340B policy changes and broadening the list of surgeries covered at ambulatory surgical centers, would generally be credit negative and hurt hospital margins.
- Changes include no longer paying more for clinic visits in off-campus hospital or provider-based department clinics compared to a physician's office...
- Proposed changes to the 340B policy could also impact certain hospitals...CMS lowered reimbursement for Part B drugs to the drug's average selling price, minus 22.5 percent from the ASP, plus 6 percent. CMS said this would save Medicare about about $1.6 billion...
- CMS has proposed adding some nonsurgical procedures to those covered at ambulatory surgical centers, which are located off-campus, but are not hospital outpatient surgery centers...
- FDA looks at incentives, manufacturing ‘interventions’ to solve drug shortages (fiercepharma.com)
The FDA will consider creating a list of “essential drugs” and financial incentives to drugmakers that manufacture them as it continues to grapple with the drug shortages that plague U.S. hospitals and caregivers...FDA Commissioner Scott Gottlieb, M.D...announced the formation of a new Drug Shortages Task Force and named Keagan Lenihan, the FDA’s associate commissioner for strategic initiatives to lead it...“I’m charging the shortages task force to delve more deeply into the reasons why some shortages remain a persistent challenge,” Gottlieb said. “The charge to this new task force is to look for holistic solutions to addressing the underlying causes for these shortages.”...The FDA is already taking steps to support new technologies that can improve manufacturing and help reduce the chance that supply disruptions will occur...the FDA may want to consider “more significant interventions” than it currently employs. “We want to make sure we aren’t discouraging investment for manufacturing drugs that are more likely to go into shortage, and thus working against our own goals." One suggestion is to grant the FDA authority to require applicants of certain drugs to conduct a “risk assessment to identify the vulnerabilities in their drug supply that could cause a shortage," and to establish risk mitigation plans in advance to address those weaknesses...
- Trump administration halts billions in insurance payments under Obamacare (reuters.com)
The Trump administration...halted billions of dollars in payments to health insurers under the Obamacare healthcare law, saying that a recent federal court ruling prevents the money from being disbursed...The Centers for Medicare and Medicaid Services, which administers programs under the Affordable Care Act, said the action affects $10.4 billion in risk adjustment payments...President Donald Trump’s administration has used its regulatory powers to undermine Obamacare after the Republican-controlled Congress last year failed to repeal and replace the law. About 20 million Americans have received health insurance coverage through the program...The payments are intended to help stabilize health insurance markets by compensating insurers that had sicker, more expensive enrollees in 2017. The government collects the money from health insurers with relatively healthy enrollees, who cost less to insure...