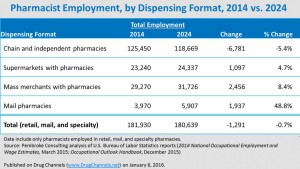
- Grim Job Outlook for Retail Pharmacists, says BLS (drugchannels.net)
The New Year is here—let’s kick it off with some good news/bad news for pharmacists...According to our...analysis of the Bureau of Labor Statistics’ new Occupational Outlook Handbook, drugstores are projected to employ about 7,000 fewer pharmacists in 2024 than they do today...The good news? Pharmacists jobs in non-retail settings—hospitals, doctor’s office, and clinics—will add more jobs than the ones lost from retail...Employment will increase at other outpatient dispensing formats, with mail pharmacies experiencing the largest percentage increase..."Demand is projected to increase for pharmacists in a variety of healthcare settings, including hospitals and clinics. These facilities will need more pharmacists to oversee the medications given to patients and to provide patient care, performing tasks such as testing a patient’s blood sugar or cholesterol…Employment of pharmacists in traditional retail settings is projected to decline slightly as mail order and online pharmacy sales increase."
- Half Of U.S. Doctors ‘Burned Out’ As Obamacare Begins Third Year (forbes.com)
The number of U.S. physicians who say they are suffering "burnout" has jumped to more than half of doctors as the practice of medicine becomes more complicated and millions more Americans gain health coverage under the Affordable Care Act...An analysis from researchers at the Mayo Clinic and the American Medical Association say doctors’ work-life balance is worsening, with the percentage of physicians who say they are suffering burnout rising to 54% in 2014 from 45% in 2011..."disturbing trend"..."Burnout and satisfaction with work-life balance among U.S. physicians are getting worse,"..."American medicine appears to be at a tipping point with more than half of U.S. physicians experiencing professional burnout...has effects on quality of care, patient satisfaction, turnover, and patient safety, these findings have important implications for society at large."
- Nevada ranks 38th in nation for overall health (rgj.com)
According to an annual report from the United Health Foundation, Nevada is ranked 38th in the U.S. when it comes to health...Nevada’s rank in 2014 was 39, so the state has improved over the past year. Here are some snapshots of how Nevada compares to national numbers for health-related topics:
- In Nevada, 17 percent of people smoke compared to the 18 percent national average.
- Drug deaths are significantly higher in Nevada, with 22.4 overdose deaths per 100,000 people compared to a 13.5 death average nationally.
- Nevada is average when it comes to the inactivity of adults. 22.5 percent of adults in Nevada are physically inactive compared with 22.6 nationally.
- Infant mortality is lower in Nevada, with 5.1 deaths per 1,000 live births compared to the 6 national average.
- In Nevada, 27.7 percent of adults are obese compared to the national average of 29.6. For diabetes, 9.6 percent of Nevadan adults have diabetes compared to 10 percent nationwide.
- For children’s vaccinations, 67.7 percent of children in Nevada are immunized compared to 71.6 nationally.
The top five healthiest states in the nation, according to the report, include Hawaii, Vermont, Massachusetts, Minnesota and New Hampshire
- Survey: Employers taking action to cut specialty drug coverage (drugstorenews.com)
Employers are taking significant action to reduce their exposure to rising costs associated with specialty medicines...Although pharmacy represents approximately 20% of employer-sponsored medical benefits costs, it is increasing at a rate that accounts for roughly half of medical cost inflation and should be a top priority for employers...The price, utilization and delivery of specialty prescription drugs, many of which require special handling or delivery, are a top pain point for employers...employers are beginning to consider new aggressive approaches... employers have added new coverage and utilization restrictions for specialty pharmacy, such as requiring prior authorization or limiting quantities based on clinical evidence... employers plan to exclude compounds from their benefit coverage...the compounding process results in higher cost and their use may not be FDA-approved in compound form, health insurers increasingly will not cover them...
- Commonwealth Fund releases its 2015 state-by-state health system scorecard (healthcareitnews.com)Aiming Higher - Results from a Scorecard on State Health System Performance (commonwealthfund.org)The good news? More states improved than worsened...The Commonwealth Fund has released "Aiming Higher," its 2015 scorecard measuring the performance of health systems state by state...Forty-two indicators are examined to arrive at the scores, measuring rates of children or adults who are uninsured, hospital patients who get information about how to handle their recovery at home, hospital admissions for children with asthma and breast and colorectal cancer deaths, among many others...The top states? Minnesota, Vermont, Hawaii, Massachusetts, Connecticut, New Hampshire and Rhode Island...Louisiana, Tennessee, Kentucky and Oklahoma ranked in the bottom quartiles, but they were among those that improved on the greatest number of indicators... key findings:
- There are wide variations in performance, with up to an eightfold difference between top- and bottom-ranked states.
- National attention may be encouraging better quality of care in hospitals and home health care settings and to more appropriate medication use in nursing homes and doctor's offices. However, declining rates of preventive care in several states signal the need for greater attention to prevention.
- Reductions in hospital readmissions accelerated in 2012, when the federal government began financially penalizing hospitals with high rates of readmissions. Rates of potentially preventable admissions to the hospital continued to fall in several states.
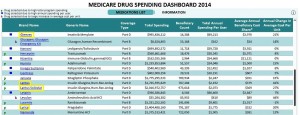
- Big Pharma’s steady double-digit price hikes cost Medicare billions (fiercepharma.com)Medicare drug costs rose sharply in 2014 (statnews.com)Medicare Drug Spending Dashboard 2014 (cms.gov)The CMS Blog: Medicare Drug Spending Dashboard (blog.cms.gov)
Sanofi, Pfizer, Novartis and peers ratchet up prices on blockbuster meds to reap big sales gains…a new report from the Center for Medicare and Medicaid Services puts some numbers to that claim. They won't resolve the debate over which price increases are "justified," but they do highlight some commonly used meds whose sales growth (grew)--and Medicare spending--depends more on rising prices than on rising demand.
- Vimovo...price hike at 543% for 2014... boost helped send spending on the drug up past $38 million from just over $7 million in 2013…patients using the drug only grew by 8%.
- Targretin...unit cost rose by 123% last year, to $145.65...CMS shelled out $73.5 million, more than double its 2013 spending…increase in patients of just 12%.
- CMS laid out $1.725 billion for Lantus last year, a $400 million increase year-over-year despite a 6% decline in patient count.
- CMS spent another $2.02 billion for Lantus Solostar, an increase of almost $700 million, or about 50% year-over-year...patient growth amounted to 13%.
- Gleevec sent CMS' unit costs up by 21% last year, to $179.93...that pushed spending per user to $69,212. The number of patients using the drug ticked upward by 5%...spending on the drug grew by 28%, to almost $1 billion.
- Lyrica...up in price...about 20%...to $4.28 per pill. Medicare spent $1.4 billion on the drug in 2014, up from just over $1 billion in 2013...patients grew by 7%.
When Sanofi, Pfizer and Novartis were raising their prices...they were fighting to fill patent-cliff sales gaps and scrambling to refill their pipelines of prospective new drugs. They were also spending billions on R&D--and on stock buybacks, dividends and other shareholder-friendly moves. Horizon and Valeant, by contrast, aren't big R&D spenders; Valeant, at least, has defended its price hikes as necessary to deliver returns to shareholders.
- Ethical Dilemmas for Health-System Pharmacists Projected to Intensify (pharmacytimes.com)
Health-system pharmacists will inevitably face growing ethical challenges as their roles in patient care continue to evolve...ethical dilemmas embedded in health-system pharmacists’ everyday practice include competing interests, limited resources due to drug shortages, and an evolving health care delivery system that has shifted their role from dispensing medications to actively participating in direct patient care...One of the hot-button ethics issues in pharmacy currently is the trend of skyrocketing prescription costs and the lack of transparency in drug pricing decisions. Extremely high prices and lagging reimbursement may preclude health-systems from providing necessary medications to all patients who would otherwise benefit..."Patient welfare is at risk when the ethical perspective in health care is smothered by business and financial perspectives,"..."Patient well-being often hinges on the ability of health professionals to heed the ethical precepts of their calling."...Pharmacists are currently vying to gain support for an expanded role in patient care in the form of provider status, which will likely be more easily garnered if they are perceived as being on the side of patient care rather than the side of business interests.
- Pharmacists ranked No. 2 in latest Gallup ethics poll (drugstorenews.com)Americans Rate Nurses Highest on Honesty, Ethical Standards (gallup.com)
Pharmacists ranked No. 2 in Gallup's 2015 Honesty and Ethics of Professions Ratings, falling behind No. 1 ranked nurses and ahead of No. 3 ranked medical doctors...This annual Gallup survey presents another data point in the strong and growing case for pharmacy patient care...those who have more first-hand experience with pharmacist-provided services feel even more strongly about their value. These positive attitudes are translating into ever-stronger bipartisan support for pro-patient and pro-pharmacy initiatives in the U.S. Congress, as well as an expansion of the pharmacists’ scope of practice in the states.
- Study: Florida’s Crackdown On ‘Pill Mills’ Is Working (forbes.com)
State officials have been cracking down on Florida’s "pill mills" over the past five year to prevent pain clinics from dispensing large quantities of prescription opioids to residents without following proper protocol–and their efforts seem to be paying off...a new study revealed that approximately 1,029 fewer people in Florida lost their lives to prescription opioid-related overdoses over a 34-month period than would have had the Sunshine State not targeted pill mills beginning in 2010...State officials passed new laws in 2010 and 2011 to curb opioid abuse, misuse and overdose in the state by establishing greater oversight over pain clinics. "These laws prohibited on-site dispensing of most prescription narcotics, prohibited advertising and increased criminal penalties for doctors and clinic owners involved drug diversion,"..."In addition, state and local law enforcement collaborated with the DEA to enforce these new laws, arresting pill mill owners, physicians and other staff, and seizing assets."...The study’s authors believe Floridians are less likely to become addicted to heroin because people are less likely to abuse prescription opioids, mainly due to the fact that they aren’t readily available in the state.
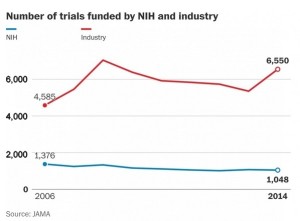
- The testing of new drugs is on the rise. Why that worries some people. (washingtonpost.com)
As the budget for the National Institutes of Health, the nation's largest funder of biomedical research, has flatlined over the past decade, the number of clinical trials funded by the federal agency has dramatically declined, a new study has found. At the same time, the number of trials funded by the pharmaceutical industry has exploded...Meanwhile, the number of NIH-sponsored trials fell from 1,376 registered on a website in 2006 to 1,048 by 2014, according to the study, which was published in the Journal of the American Medical Association. Industry-sponsored trials grew by about 2,000 over the same period, reaching 6,550 registered in 2014...More trials is generally a good thing...because it means that more new drugs, devices or other treatments are being tested. But the decline in federally funded trials concerns public health researchers, because federally funded trials are independent, often intended to compare drugs or other treatments instead of simply to show that a product works and should gain federal approval…there are many areas of deserving research...there may need to be a formal discussion of how research dollars are spent. A reasonable way to begin...is to look at the burden of a particular disease and allotting research dollars to those that have the greatest effect on mortality and disability...