- The co-pay card debate simmers, as payers push back (mmm-online.com)
Any program that puts more greenbacks in patients' pockets in this post-recession economy has to be viewed as a good one, right? Alas, it depends on the person you ask...Devised to shoulder some of the cost burden of prescription drugs, manufacturer co-pay card programs have been tied to improved adherence rates and reduced barriers to the discounted medications. At the same time, payers — insurers and PBMs alike — are crying foul...While some industry veterans sing the praises of co-pay assistance programs, others are eager for a more evenhanded and efficient solution that will achieve the same degree of cost savings. In fact, the co-pay card appears to be stirring the controversy pot more than ever. Indeed, the question seems to have become: What will make it boil over?
- Obama Declares ACA Success in JAMA, Calls for Taking Steps to Reduce Drug Costs (ajmc.com)United States Health Care ReformProgress to Date and Next Steps (jama.jamanetwork.com)
President Barack Obama today declared in a special issue of JAMA that the Affordable Care Act has worked, both by driving down the share of Americans without health coverage and by "transforming healthcare payment systems," that are improving quality and reining in spending...The president’s article, "United States Health Care Reform: Progress to Date and Next Steps," highlights what he sees as the achievements of the signature law often called "Obamacare," while calling for more work to cut prescription drug prices and fill gaps where market competition is lacking, perhaps with a "public option."..."Americans can now count on access to health coverage throughout their lives, and the federal government has an array of tools to bring the rise of healthcare costs under control," Obama writes. "However, the work toward a high-quality, affordable healthcare system is not over."
- Insurer Obamacare Losses Reach Billions Of Dollars After Two Years (forbes.com)
After two years offering uninsured Americans subsidized products on public exchanges, health insurance companies have been hard-pressed to find financial success in this segment of the Affordable Care Act with losses reaching billions of dollars for the industry...UnitedHealth Group lost more than $720 million on its public exchange business last year and United is a small player in this market compared to Anthem, which operates Blue Cross and Blue Shield plans in 14 states, and said money-losing Obamacare plans caused profits to fall 64 percent in the fourth quarter. Aetna, which hopes to finalize its acquisition of Humana later this year, said last week individual coverage sold under the health law "remained unprofitable" last year...For insurers, the problem has largely been a major increase in medical expenses from these new patients, who were previously uninsured. From an actuarial standpoint, the health plans say they didn’t know what they would be getting and therefore needed more healthy people to buy premiums to cover the costs of the sick.
- National Health Spending In 2014: Faster Growth Driven By Coverage Expansion And Prescription Drug Spending (content.healthaffairs.org)
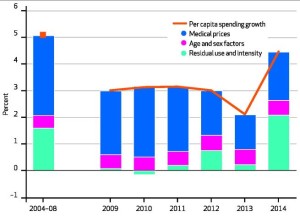
Factors Accounting For Growth In Per Capita National Health Expenditures, Selected Calendar Years 2004–14
US health care spending increased 5.3 percent to $3.0 trillion in 2014. On a per capita basis, health spending was $9,523 in 2014, an increase of 4.5 percent from 2013. The share of gross domestic product devoted to health care spending was 17.5 percent, up from 17.3 percent in 2013. The faster growth in 2014 that followed five consecutive years of historically low growth was primarily due to the major coverage expansions under the Affordable Care Act, particularly for Medicaid and private health insurance, which contributed to an increase in the insured share of the population…growth in total retail prescription drug expenditures accelerated sharply, increasing 12.2 percent to $297.7 billion…The strong growth in prescription drug expenditures in 2014 was caused by increased spending on new medicines, a smaller impact from patent expirations than in previous years, and price increases for brand-name drugs. The single largest driver of growth in specialty drug spending in 2014 was the impact of new treatments for hepatitis C, which contributed $11.3 billion in new spending.
The Affordable Care Act | Factors Accounting For Growth | Revisions To The National Health Expenditure Accounts | Sponsors Of Health Care | Private Health Insurance | Medicaid | Medicare | Out-Of-Pocket Spending | Retail Prescription Drugs | Hospital Care | Physician And Clinical Services
- The Justice Department Fights Health Insurers Trying To Survive The Obamacare Wasteland (forbes.com)
Most health policy experts knew, and many warned, that the Affordable Care Act would lead to massive consolidation in the health care industry, including hospitals, physicians’ practices, and especially health insurers. Now the Justice Department is pushing back by opposing the mergers of four large health insurers—Aetna with Humana and Anthem with Cigna —as they try to survive the Obamacare wasteland...The Obama administration defended its opposition by claiming the mergers would reduce competition. Attorney General Loretta Lynch explained, "If allowed to proceed, these mergers would fundamentally reshape the health insurance industry." That’s rich, since nothing has reshaped the health insurance industry more than Obamacare—and by design...Obama officials dismiss the health insurer losses, claiming that many of the insurers are still profitable. But that’s because health insurers often have several lines of business, some of which may be profitable even as they lose hundreds of millions of dollars selling in Obamacare exchanges. No responsible board of directors will let such losses continue indefinitely...Policyholders will likely be receiving the notice that their premiums are rising or policy is being canceled in September or October—just before the election...
- Obamacare Was Going to Lower Health Care Costs. What Actually Happened. (dailysignal.com)
Has Obamacare Reduced Costs?...Those family cost savings, of course, have not materialized...the health care cost curve is still on an upwardly mobile trajectory...Centers for Medicare and Medicaid Services data show that total per capita health insurance spending will rise from $7,786 in 2016 to $11,681 in 2024. Looking at the future of employer-based health insurance costs, the Congressional Budget Office (CBO) projects that job-based premiums are poised to increase by almost 60 percent between now and 2025...the Affordable Care Act...calls for sustained payment cuts to the popular Medicare Advantage program. It also has scheduled some big Medicare payment reductions over the next ten years for hospitals, nursing homes, home health agencies and even hospice care programs...Medicare trustees report that, if policymakers really go through with these Affordable Care Act provisions, 50 percent of America’s hospitals, 70 percent of the nation’s nursing homes and 90 percent of the nation’s home health agencies will be operating in the red in the next 24 years...This...will jeopardize seniors’ access and quality of care.
- CMS final rule addresses decades-long Medicaid reimbursement issue (drugstorenews.com)
The end of what has become a decades long battle around fair reimbursement for Medicaid programs and pharmacy appears to be in sight...the Centers for Medicare & Medicaid Services issued the Covered Outpatient Drugs final rule with comment that addresses key areas of Medicaid drug reimbursement and changes made to the Medicaid Drug Rebate Program by the Affordable Care Act. According to a fact sheet published by CMS, this final rule assists states and the federal government in managing drug costs, establishes the long term framework for implementation of the Medicaid drug rebate program and creates a more fair reimbursement system for Medicaid programs and pharmacies...the final rule is designed to ensure that pharmacy reimbursement is aligned with the acquisition cost of drugs and that the states pay an appropriate professional dispensing fee. The final rule:
- Creates an exception to the FUL calculation, which allows for the use of a higher multiplier than 175% to calculate the FUL based on acquisition costs for certain multiple source drugs;
- Establishes actual acquisition cost as the basis by which states should determine their ingredient cost reimbursement so payments are based on a more accurate estimate of the prices available in the marketplace, while still ensuring sufficient beneficiary access;
- Implements the use of the term professional dispensing fee to ensure that the dispensing fee paid to pharmacies reflect the cost of the pharmacist’s professional services and cost to dispense the drug product to a Medicaid beneficiary;
- Clarifies that states are required to evaluate the sufficiency of both the ingredient cost reimbursement and the professional dispensing fee reimbursement when proposing changes to either of these components; and
- Requires states to specify in the Medicaid state plan that reimbursement methodology to pharmacies that purchase drugs through the Federal Supply Schedule and the 340B Drug Pricing Program is consistent with overall AAC requirements.
- Medical groups push to water down requirements for disclosing industry ties (statnews.com)S. 2978: Protect Continuing Physician Education and Patient Care Act (govtrack.us)OpenPayments (cms.gov)
Nearly 100 national and state medical societies from around the United States are backing a Senate bill (Protect Continuing Physician Education and Patient Care Act, (SB 2978) that would exempt drug and device makers from reporting payments made to doctors for receiving continuing medical education...sessions, medical journals, or textbooks. Among them are the American Medical Association and the American College of Cardiology...The move is the latest push in a long-running effort to roll back requirements for reporting such payments to a federal database, which tracks financial relationships between companies and physicians. Known as OpenPayments, the database was launched...in response to concerns that financial ties between drug firms and device makers and doctors may unduly influence medical practice and research. It was included in the Sunshine Act provision in the Affordable Care Act. A recent analysis found that payments can affect prescription rates...
- ACA ‘Savings’: Paying Doctors And Hospitals Bonuses To Deny Care To Patients (forbes.com)
...one of the lesser-known provisions of the ACA (Affordable Care Act) calls for the federal government to pay physicians and hospitals bonuses if they deny health care to seniors and the disabled...Section 3022 of the ACA establishes the Medicare Shared Savings Program. The MSSP establishes the notion of Accountable Care Organizations. These are groups of health care providers (hospitals, physicians, other providers) who join together for purposes of a obtaining bonus payments based on their participation in the MSSP and Medicare fee-for-service incentive program...ACOs are paid to "reduce costs" for treating their patients...For patients assigned to ACOs, the ACO receives bonus payments based on the total amount Medicare pays for care of those patients. That total includes all care those patients receive from all providers – specifically, including providers who are not members of the ACO. Bonuses are based on reducing total costs relative to what would be expected risk-adjusted cost based on each patient’s health status...Because this program is part of Medicare’s fee-for-service system, "reduce costs" means "reduce services" – that is, "give patients less health care."...the ACO program encourages hospitals and physicians...to encourage patients to use less health care...It is highly ironic that a law proposed, in part, because of the allegation health insurance companies were increasing their profits by denying care to patients – is now the means by which the federal government pays physicians and hospitals bonuses to, in effect, deny care to patients...
- How Stable Are the ACA Marketplaces? (commonwealthfund.org)
The news that UnitedHealth Group is considering leaving the new health insurance marketplaces established under the Affordable Care Act has prompted some concern about the their long-term viability...United Health Group’s possible departure is not really the issue. The insurer was a minor player in the individual market before the ACA passed, and currently covers only about 5 percent of marketplace enrollees…together with a few other developments, such as the failure of COOPs, the UnitedHealth Group announcement raised the fundamental question of whether the ACA marketplaces are enrolling sufficient numbers of people to ensure a well-balanced risk pool of healthy people and those with health problems. A pool where a majority of people have health problems could lead to higher premiums over time and destabilize marketplaces.