- Nevada’s already slim physician workforce may grow slimmer with patients slow to return to doctor’s offices (thenevadaindependent.com)
A majority of Nevada doctors believe they can only keep their doors open for another two to six months unless the volume of patients trickling back into their offices significantly increases, according to a new survey from the American Medical Association...Ten percent of physicians in Nevada reported layoffs, 15 percent reported pay cuts, 20 percent reported temporary furloughs and 30 percent reported a reduction in staff hours, while 55 percent reported none of those changes, according to preliminary results from the survey, which Dr. Ron Swanger, president of the Nevada State Medical Association, presented to the Patient Protection Commission...READ MORE
- 5 ways to streamline prior authorization, improve outcomes (fiercehealthcare.com)2017 AMA Prior Authorization Physician Survey (ama-assn.org)
Physicians say they face long wait times for insurers to process prior authorizations and the delays can negatively impact patient outcomes...The American Medical Association surveyed 1,000 physicians, and 64% said they wait at least one business day for insurers to decide on prior authorization. Nearly one-third (30%) said they wait at least three business days for decisions...The vast majority of physicians surveyed said that lag time can have serious consequences for patients; 92% said the prior authorization process can lead to delays in access to care, and 78% said that waiting for a decision from insurers "sometimes, often or always" causes patients to abandon certain treatments entirely...The AMA survey illustrates a critical need to help patients have access to safe, timely and affordable care, while reducing administrative burdens that take away from patient care...Six major industry groups—including America's Health Insurance Plans and the AMA—joined forces to improve the prior authorization process. The groups agreed to five steps:
1. Reduce the number of healthcare professionals subject to prior authorization requirements based on their performance, adherence to evidence-based medical practices or participation in a value-based agreement with the health insurance provider.
2. Review the services and medications that require prior authorization on a regular basis and eliminate requirements for therapies that no longer warrant them.
3. Improve communication between health insurance providers, healthcare professionals and patients to minimize delays in care and ensure clear prior authorization requirements, rationale and changes.
4. Protect the continuity of care for patients on an ongoing active treatment or a stable treatment regimen when there are changes in coverage, insurance providers or prior authorization requirements.
5. Accelerate industry adoption of national electronic standards for prior authorization and improve transparency of formulary information and coverage restrictions at the point-of-care. - Medical groups push to water down requirements for disclosing industry ties (statnews.com)S. 2978: Protect Continuing Physician Education and Patient Care Act (govtrack.us)OpenPayments (cms.gov)
Nearly 100 national and state medical societies from around the United States are backing a Senate bill (Protect Continuing Physician Education and Patient Care Act, (SB 2978) that would exempt drug and device makers from reporting payments made to doctors for receiving continuing medical education...sessions, medical journals, or textbooks. Among them are the American Medical Association and the American College of Cardiology...The move is the latest push in a long-running effort to roll back requirements for reporting such payments to a federal database, which tracks financial relationships between companies and physicians. Known as OpenPayments, the database was launched...in response to concerns that financial ties between drug firms and device makers and doctors may unduly influence medical practice and research. It was included in the Sunshine Act provision in the Affordable Care Act. A recent analysis found that payments can affect prescription rates...
- The testing of new drugs is on the rise. Why that worries some people. (washingtonpost.com)
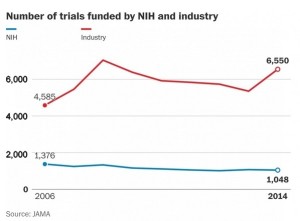
As the budget for the National Institutes of Health, the nation's largest funder of biomedical research, has flatlined over the past decade, the number of clinical trials funded by the federal agency has dramatically declined, a new study has found. At the same time, the number of trials funded by the pharmaceutical industry has exploded...Meanwhile, the number of NIH-sponsored trials fell from 1,376 registered on a website in 2006 to 1,048 by 2014, according to the study, which was published in the Journal of the American Medical Association. Industry-sponsored trials grew by about 2,000 over the same period, reaching 6,550 registered in 2014...More trials is generally a good thing...because it means that more new drugs, devices or other treatments are being tested. But the decline in federally funded trials concerns public health researchers, because federally funded trials are independent, often intended to compare drugs or other treatments instead of simply to show that a product works and should gain federal approval…there are many areas of deserving research...there may need to be a formal discussion of how research dollars are spent. A reasonable way to begin...is to look at the burden of a particular disease and allotting research dollars to those that have the greatest effect on mortality and disability...
- Punishing Patients Won’t Reduce Opioid Deaths (reason.com)
Barbara McAneny, president of the American Medical Association, recently described a patient with metastatic prostate cancer who tried to kill himself after he could not get the medication he was prescribed for bone pain because...his insurer...denied coverage...my patient nearly died of an underdose...McAneny was talking about the suffering caused by government pressure to reduce opioid prescriptions, which has led to denials of treatment and arbitrary dose reductions...A Medicare rule that take effect on January 1 will compound that problem...
- No new antidepressants in sight despite growing need, experts warn (finance.yahoo.com)
It is likely to be at least 10 years before any new generation of antidepressants comes to market, despite evidence that depression and anxiety rates are increasing across the world…The depression drug pipeline has run dry partly due to a "failure of science"...but also due to big pharma pulling investment out of research and development in the neuroscience field because the profit potential is uncertain...risk aversion was understandable given uncertain returns and the approximately billion dollar cost of developing and bringing a new drug to market...Treatment for depression usually involves either medication, some form of psychotherapy, or a combination of both. But up to half of all people treated fail to get better with first-line antidepressants, and around a third of patients are resistant to relevant medications...
- Opinion: The AMA is wrong about banning drug ads (statnews.com)
...American Medical Association recently called for a ban on advertising prescription drugs and medical devices directly to consumers. The effort is largely symbolic...But doctors resent the increasing pressure the ads place on them to write prescriptions out of concern patients will switch physicians...they argue that many ads aimed at consumers promote more expensive medicines...and pushes patients to ask for products that either they may not need or is not right for them. This approach is, at best, misguided, and, at worst, ignores the benefits of direct-to-consumer advertising for patients...DTC advertising increases awareness of health problems and leads to a better informed and educated patient who can engage their physician in a dialogue rather than a monologue...So what’s really going on here?...insurers are taking more prescription writing power away from doctors. They first want patients to try generic medications which now make up 88 percent of all available prescription drugs. Second, higher patient copayments for office visits and insurance mean consumers are “shopping” for health care and health care treatments...This makes doctors very uncomfortable. Even with all these changes, research continually validates the notion that patients view their doctors as the gatekeepers to their prescription medicines...DTC advertising leads patients to their health care providers and, depending on the health condition, does not lead to high-priced unnecessary scripts. The AMA should reach out and work with pharma to improve DTC marketing, not request a ban on all DTC ads.
- Backed by medical groups, value-based payments for opioid addiction treatment could be imminent (fiercehealthcare.com)PATIENT-CENTERED OPIOID ADDICTION TREATMENT (P-COAT) (asam.org)
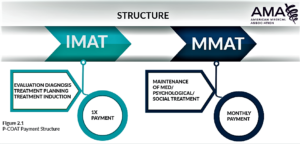
Two medical associations have announced a collaborative value-based payment model for opioid addiction treatment...The payment model, announced by the American Society of Addiction Medicine and the American Medical Association, is aimed at improving care coordination and lowering healthcare spending by reducing costly emergency department visits and hospitalizations...The model increases utilization of and access to medications for opioid treatment, combining them with the appropriate level of medical, psychological and social support services which can be delivered at multiple providers…The model is for outpatient care only...a basic version of the model is already in operation with Optum…the groups have discussed the model with officials at the Centers for Medicare & Medicaid Services, as well as its innovation center, which is responsible for new demonstration programs.
- AMA embraces value-based drug pricing (modernhealthcare.com)
The nation's largest physician organization is supporting value-based pricing for medications...The American Medical Association...announced it supports initiatives...aimed at changing the fundamentals of prescription drug pricing without compromising patient outcomes and access...Its new policy...seeks to blunt growing pharmaceutical spending rates...by incorporating a balance of benefits and cost when pricing drugs. The organization believes prices should be set by objective, independent agencies that use evidence and data. Processes to set those prices should be transparent, not burden physicians or patients and maintain affordability for patients...The new AMA policy acknowledges the carte blanche approach to drug pricing needs to change to align with the health system's drive for high-quality care based on value...This transformation should support drug prices based on overall benefit to patients compared to alternatives for treating the same condition. We need to have the full picture to assess a drug's true value to patients and the health care system...
- Half Of U.S. Doctors ‘Burned Out’ As Obamacare Begins Third Year (forbes.com)
The number of U.S. physicians who say they are suffering "burnout" has jumped to more than half of doctors as the practice of medicine becomes more complicated and millions more Americans gain health coverage under the Affordable Care Act...An analysis from researchers at the Mayo Clinic and the American Medical Association say doctors’ work-life balance is worsening, with the percentage of physicians who say they are suffering burnout rising to 54% in 2014 from 45% in 2011..."disturbing trend"..."Burnout and satisfaction with work-life balance among U.S. physicians are getting worse,"..."American medicine appears to be at a tipping point with more than half of U.S. physicians experiencing professional burnout...has effects on quality of care, patient satisfaction, turnover, and patient safety, these findings have important implications for society at large."