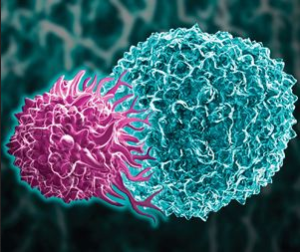
- Medicare to cover expensive cancer cell therapies (reuters.com)
...Centers for Medicare and Medicaid Services...said it has finalized a decision to cover expensive cancer cell therapies sold by Gilead Sciences Inc and Novartis AG...CMS...said it will cover the U.S. Food and Drug Administration-approved therapies when provided in healthcare facilities that have programs in place to track patient outcomes...The nationwide decision clears up “a lot of confusion” about coverage and will help patients get access to the novel therapies...CMS Administrator Seema Verma said...READ MORE
- CMS finalizes site neutral payment rule (healthcarefinancenews.com)
The Centers for Medicare and Medicaid Services has finalized site neutral payments in the hospital outpatient prospective payment system and ambulatory surgical center payment system rule...CMS is using site neutral payments to level the playing field between what physician offices and hospital outpatient departments are paid for certain clinical visits...In addition...CMS is expanding its 340B policy by extending the payment change to additional off-campus provider-based hospital outpatient departments that are paid under the physician fee schedule...Today's rule advances competition...for providers so they can compete for patients on the basis of quality and care...The final policies remove unnecessary and inefficient payment differences so patients can have more affordable choices and options.
- Moody’s: CMS proposed changes to Medicare’s outpatient prospective payment system could hurt hospitals (healthcarefinancenews.com)
...the Centers for Medicare and Medicaid Services' proposed changes to outpatient services, including site neutral clinic visits, 340B policy changes and broadening the list of surgeries covered at ambulatory surgical centers, would generally be credit negative and hurt hospital margins.
- Changes include no longer paying more for clinic visits in off-campus hospital or provider-based department clinics compared to a physician's office...
- Proposed changes to the 340B policy could also impact certain hospitals...CMS lowered reimbursement for Part B drugs to the drug's average selling price, minus 22.5 percent from the ASP, plus 6 percent. CMS said this would save Medicare about about $1.6 billion...
- CMS has proposed adding some nonsurgical procedures to those covered at ambulatory surgical centers, which are located off-campus, but are not hospital outpatient surgery centers...
- CMS Puts Off Decision on Lowering Drug Prices Patients Pay at the Pharmacy (ptcommunity.com)
The Centers for Medicare and Medicaid Services has laid out a bevy of initiatives that officials said would reduce drug prices for patients covered by the Medicare Part D prescription drug program—but they have made no decisions yet...That issue is whether the discounts that pharmacy benefit managers negotiate for drugs—the “rebates” that lawmakers have been raising questions about in recent months—as well as other fees, should go toward lowering the price that a patient pays at the pharmacy...“While we are not finalizing any policy in this area at this time, we appreciate the detailed submissions from stakeholders, and we are evaluating these comments as we consider future proposals,” said CMS Administrator Seema Verma...It’s unclear whether lowering the amount of money that the patient pays at the pharmacy would actually lower the total amount of health care spending. According to an analysis by CMS that was part of the proposed rule in November, patients would indeed pay less, but the government would pay more...
- Trump administration proposes rule requiring hospitals to publish the prices negotiated with insurers (cnbc.com)
The Trump administration is proposing a rule that would require hospitals to publish the prices that are negotiated with insurers or risk being fined...The proposed rule...would apply to the roughly 6,000 hospitals that accept Medicare. Hospitals could be fined up to $300 a day if the standard and negotiated prices for services are not posted online...Starting this year, the administration required hospitals to publish list prices, or the sticker price. That does not reflect what someone might pay with insurance. The proposed rule would go a step further and require hospitals to also post the prices various insurance plans pay...“We’re trying to change the paradigm here,” Centers for Medicare & Medicaid Services Administrator Seema Verma said...“We’re trying to ensure we have a competitive free market where providers can compete on cost and quality and patients have the information they need to seek high-quality providers.”...READ MORE
- CMS proposes rule to streamline Medicare compliance (fiercehealthcare.com)
CMS took the latest step in its Patients over Paperwork initiative...issuing a proposed rule that would eliminate or update a slew of regulations deemed “unnecessary, obsolete or excessively burdensome” on providers...Should the rule be finalized, the Centers for Medicare & Medicaid Services estimates that it would save providers $1.12 billion each year and eliminate millions of hours in administrative time. Through 2021, CMS projects $5.2 billion in total savings and 53 million hours of administrative burden eliminated...Much of the rule focuses on streamlining CMS’ conditions of participation and conditions for coverage, which the agency says will allow providers to operate more fluidly and efficiently without impacting patient safety and care quality. Some of the key changes the rule proposes include:
- Allowing health systems to use an integrated quality assessment and improvement platform across all their member hospitals.
- Creating a simpler process for providers to order portable X-ray machines and updating the requirements for portable X-ray technologists.
- Easing requirements for hospitals and ambulatory surgery centers for conducting physicals and collecting patient histories ahead of procedures.
- Eliminating a requirement for critical access hospitals to disclose people with a financial interest in the facility, as CMS also obtains that information outside of compliance with the conditions of participation.
- Experts weigh in on CMS’ big changes to clinical documentation, EHRs and interoperability (healthcareitnews.com)
Industry groups like easier quality reporting and advance applications of telehealth, but some say docs shouldn't have to make expensive EHR upgrades for 2019..."historic changes" announced...by the Centers for Medicare & Medicaid Services, promising big adjustments to its policies around the Physician Fee Schedule and the Quality Payment Program, already have the healthcare industry talking...CMS says it wants to incentivize the use of and access to virtual care and telehealth, to ease the quality reporting burden on physicians by focusing on the most important and impactful measures...also wants to spur better information sharing among healthcare providers, regardless of what electronic health record vendor they happen to use...CMS notes that these proposals will modernize Medicare payment policies to promote access to virtual care, saving Medicare beneficiaries time and money while improving their access to high-quality services no matter where they live...the new proposal would "help shift the nation’s electronic documentation away from overly long, form-driven, hard-to-read documents written primarily to satisfy billing requirements to what it was originally intended for – providing high- quality care to patients."...
- CMS unveils CAR-T proposal, with emphasis on patient outcomes (biopharmadive.com)
Under a proposal...Medicare would cover CAR-T cell therapies through a Centers for Medicare and Medicaid Services pathway known as Coverage with Evidence Development...The proposal holds a mix of provisions, including that patients must be monitored for at least two years post-treatment. Hospitals administering CAR-T therapy, whether through inpatient or outpatient care, must participate in a CMS-approved registry that collects data on patient outcomes and characteristics and then compares that data to what's been seen in pivotal clinical trials of the therapy or standard of care treatment...Hospitals and clinicians would track certain clinical data elements at baseline, at treatment, and then at three-month, six-month, one-year and two-year follow ups following administration...
- How Can Medicare Save A Billion Bucks? Use Generics (ptcommunity.com)Medicare Spending on Brand-name Combination Medications vs Their Generic Constituents (jamanetwork.com)
In 2016, the cost difference between the amount that the Medicare Part D drug program spent on brand-name combination medications and the estimated cost for generic constituents for the same number of doses was $925 million, according to an investigation in the Journal of the American Medical Association...a retrospective analysis of Medicare drug spending from 2011 through 2016, looked at 29 brand-name oral combination medications, separated into three categories: medications that were available in generic form at identical doses; generic medications available at different doses; and therapeutically equivalent generic substitutes. The savings for all three categories was in the millions of dollars, with the largest discrepancy (an estimated $471 million) seen with the therapeutically equivalent generic substitutes. The authors also found that for the 10 most costly combination products that were available throughout the entire study period, the listed Medicare spending could have been an estimated $2.7 billion lower if the generic constituents had been prescribed.
- Integrating medication management with its EHR helped one hospital beat CMS expectations (healthcareitnews.com)
King's Daughters Medical Center...found it challenging to provide an accurate, verifiable home medication record for its providers to trust as they made important decisions about existing medications both during an inpatient visit and after discharge...King's Daughters now uses external medication history from pharmacy fill data as well as insurance claims data, provided by vendor DrFirst, to complement verification and push the information to the providers...While it is not intended as a replacement for the patient/family interview, its integration into the electronic health record greatly augments the conversation and can prompt a patient to include easily forgotten information...This reduces the risk of prescription loss and makes the process more efficient for the patient while ensuring the health record is updated in advance of future visits...King's Daughters is required to report its performance on both medication reconciliation (with a threshold goal of 50 percent) and e-prescription (10 percent) to the Centers for Medicare and Medicaid Services...most recent reporting period, Q4 2017, our stats were 77 percent and 52 percent, respectively...integrating medication management tech into the EHR also helped King’s Daughters more effectively retrieve historical data and deliver that information to providers to facilitate new prescriptions in a trustworthy manner that both reduces errors and the abuse of controlled substances...