- CMS Unveils Patient Data Access Initiatives (healthleadersmedia.com)
The Federal government...unveiled two initiatives designed to improve patients' access and control over their personal electronic medical records, and also pledged to overhaul Meaningful Use and refocus on data interoperability and ease of use among providers...Under the MyHealthEData initiative, patients will have access to their complete electronic health record, which they can take from doctor to doctor, choose the provider they want, and give that provider secure access to their data, leading to greater competition and reducing costs, the Centers for Medicare & Medicaid Services said...Under a second initiative, Medicare has launched Blue Button 2.0, which allows traditional Medicare beneficiaries to access and share personal health data in a universal digital format, and connect claims data to the secure applications, providers, and services they trust...CMS Administrator Seema Verma unveiled the initiatives...at the annual conference of the Healthcare Information and Management Systems Society...CMS is also taking an aggressive stance against data blocking...it is the priority of this administration to ensure that every patient and their doctor can receive free and timely access to their electronic data,"...
- AHIP thanks CMS for adding flexibility in 2019 Medicare Advantage and Part D rule (healthcarefinancenews.com)
New proposed rule offers insurers more plan flexibility and eases regulations...The proposed rule released last week by the Centers for Medicare and Medicaid Services would strengthen and improve the Medicare Advantage and Part D programs...CMS's proposed 2019 Medicare Advantage and Part D rule offers insurers greater flexibility in reporting and makes changes to how star ratings are calculated...Star ratings determine bonuses for insurers. Another plus for plans that have an overall 5-star rating is the ability to offer a year-round open enrollment period for Medicare Advantage...The rule has an open enrollment period for MA plans of Jan. 1 through March 31, 2019. It allows enrolled individuals to make a one-time election to go to another plan or to original Medicare...The proposed rule would get rid of artificial limits on the variety of plans an insurer can offer in a certain region, ease the medical loss ratio, allow for more tailored benefits and would revise regulations for maximum out-of-pocket limits, among other changes.
- Following EpiPen controversy, federal watchdog to review Medicaid rebates (statnews.com)
A government watchdog agency is conducting three new reviews of the Medicaid Drug Rebate Program to determine the extent to which drug companies are properly paying required givebacks to the health care program...Under the Medicaid Drug Rebate Program, companies must accurately report — and pay — a rebate on drugs paid for by the agency...The ruckus erupted because Mylan reported EpiPen as a generic product for nearly a decade. This is an important distinction, because classifications are used to determine the size of rebates...are lower for generics — 13 percent versus 23 percent for a brand-name product...The more we learn about the misclassifications, the more we know this program is in dire need of proper oversight...It’s unclear whether CMS took any action between 2009 and now to get the EpiPen classification back on track after being told about the misclassification...
- Implications of final AMP rule for community Rx (chaindrugreview.com)
On February 1, 2016, the Centers for Medicare & Medicaid Services released its Final Rule interpreting the provisions of the 2010 health care reform law that address the Medicaid Drug Rebate Program. While much of the Final Rule speaks to drug manufacturer rights and responsibilities in the MDRP, significant portions are directly applicable to chain drug stores...the Final Rule addresses (a) reimbursement for multisource drugs dispensed to Medicaid patients, (b) changes in the Average Manufacturer Price (AMP) that will impact pharmacy reimbursement for multisource products, (c) reimbursement for single-source drugs dispensed to Medicaid patients and (d) changes to the dispensing fees pharmacies will receive for dispensing drugs to Medicaid patients...An overarching theme expressed in the Final Rule is CMS’ desire to move states away from their historic practice of overpaying for ingredient cost while simultaneously underpaying for dispensing fees...If the Final Rule plays out as anticipated, in the coming year ingredient cost reimbursement will fall for single- and multiple-source products, but dispensing fees will rise...This reflects a desired shift away from a "spread-based" model of pharmacy Medicaid participation toward a "service-based" model. It’s currently unclear if the increased fee income to pharmacies will balance the lost reimbursement revenue.
- Multisource product ingredient cost reimbursement
- Changes in AMP affecting multisource drug reimbursement
- Single-source product ingredient cost reimbursement
- Medicaid pharmacy dispensing fees
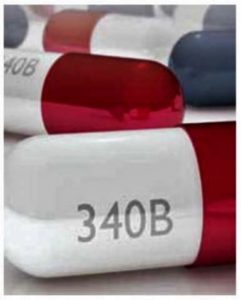
- Report: Medicare Part B Payment Hikes Could Offset 340B Cuts for Many Hospitals (ptcommunity.com)
...some dispute...findings on the controversial cuts...Increased reimbursements under Medicare Part B overall could offset potential losses for hospitals under changes to the 340B discount program, according to a new analysis...consulting firm Avalere Health analyzed hospital-level data from the Centers for Medicare and Medicaid Services on reimbursements in 2017 and 2018 and found that 85% of hospitals would receive higher Part B payouts that would minimize the reductions from cuts to 340B discounts...CMS finalized changes to 340B in November, changing its payment rate to 22.5% less than the list price for medication. Previously, it had paid up to 6% more than the list price under the program, and the cuts could equal $1.6 billion in lost payments...Rural hospitals would especially benefit from CMS’ increased Part B payouts, according to Avalere, as those facilities will net an average increase of 2.7%. Urban hospitals will see a 1.4% net increase...The 340B program wasn’t always controversial, but in recent years lawmakers and pharmaceutical companies have expressed concern that too many hospitals have enrolled, taking advantage of the program’s discounts. A study...suggests that hospitals have snapped up physician practices in areas like oncology to boost their 340B discounts but don’t often invest those savings in improving care for low-income patients.
- Understanding CMS’s Surprising Reimbursement Cut for 340B Hospitals (drugchannels.net)
Centers for Medicare & Medicaid Services shocked everyone with a proposal altering a small part of the 340B Drug Pricing Program. CMS proposed reducing reimbursement for certain Medicare Part B drugs purchased by 340B-eligible hospitals: from Average Sales Price plus 6% to ASP minus 22.5%. Hospitals will also have to identify 340B claims with a new modifier...CMS explains its rationale for reducing reimbursement to hospitals. It references key studies from the Office of Inspector General, the Government Accountability Office, and the Medicare Payment Advisory Commission...The new ASP-22.5% reimbursement figure is based on a MedPAC study. It estimated that hospitals in the 340B program receive a minimum discount of 22.5% of the Average Sales price (ASP) for drugs paid under the outpatient prospective payment system…Three important items to note:
- The proposal would reduce patients’ coinsurance obligations.
- Manufacturers would not gain from this proposal. CMS designed the proposal to be budget neutral.
- The proposal does not address contract pharmacies.
- Humana’s slashed Medicare rating may signal higher bar for all insurers (cnbc.com)
Humana says it plans to fight the Obama administration over a large reduction in the ratings of its 4-star Medicare Advantage plans for coverage starting in 2018...Star ratings are a key quality measure under Medicare, and lower ratings could result in reduced reimbursement rates for Humana...Not having 4-stars on a significant portion of your plans will hurt you financially because you will not be able to achieve the bonus reimbursement that higher rated plans receive…The company said issues resulting in reduced stars included delays in resolving enrollee complaints over claims...Clearly Humana is going to fight this...it's too early to determine what the real impact of the star rating reduction could be on Humana's earnings in 2018...They're raising the bar, in the sense that it is becoming increasingly demanding...to get the highest ratings on Medicare plans...In other words, insurers are not getting worse, but rather facing tougher comparisons...The good news is that the quality of everyone is improving, but [CMS] still wants to mark on a curve… so, by definition, not everyone can be a five-star...
- Meaningful Measures specifics emerge: CMS program will track 18 areas (healthcareitnews.com)
The Centers for Medicare and Medicaid Services...offered further insight into how the Meaningful Measures program works...deputy director of CMS' Center for Clinical Standards and Quality, said the initiative to streamline quality reporting was launched in recognition that "there's a fine line between being helpful and being a hindrance."...CMS has heard the feedback from industry stakeholders that there are too many often-overlapping quality measures...Tracking these measures does not always lead to better outcomes for patients...there are two key problems CMS wants to solve with Meaningful Measures...The first is to focus on the highest-priority measures for quality reporting and quality improvement. The second...is to improve the agency's communications with patients, clinicians and stakeholders about what measures they should be paying most attention to...the important concepts we want every measure to be filtered through...Those are: reduce regulatory burden, improve access for rural communities, achieve cost savings, safeguard public health, track to measurable outcomes and impact and eliminate disparities...Those principals...represent the guiding framework for 18 different Meaningful Measure areas that CMS wants health systems to prioritize – they're further grouped under six thematic headings:
- Make Care Safer by Reducing Harm Caused in the Delivery of Care
- Strengthen Person and Family Engagement as Partners in their Care
- Promote Effective Communication and Coordination of Care
- Promote Effective Prevention and Treatment of Chronic Disease
- Work with Communities to Promote Best Practices of Healthy Living
- Make Care Affordable
- Industry paid $8.2B to docs, hospitals last year (biopharmadive.com)
Drug and device makers collectively made nearly $8.2 billion in payments to physicians and teaching hospitals in the U.S. last year, according to data made public by the Centers for Medicare and Medicaid Services last week...Payments for research made up more than half of the total, which also includes money given to doctors and hospitals for expenses like travel, gifts, speaking fees and meals. The $8.2 billion recorded last year was a notch higher than 2015's total and $320 million more than 2014's figure...Among the ranks of big pharma...Roche spent the most — a princely $586 million in payments. Novartis and Pfizer were close behind with more than $475 million each, although both made more research-related payments than Roche did...The data gives a snapshot of the enormous sums of money paid by the drug and device industries to doctors and hospitals. Most of the money goes towards research, payments for things like enrolling patients into new clinical studies or study implementation. Research payments can also include direct compensation to doctors…CMS began tracking payments in 2013 as part of changes to federal law through the Affordable Care Act, with 2016 marking the third full year of the program...
- Mylan to pay $465 million to settle claims of shortchanging Medicaid (statnews.com)
Mylan reached a $465 million settlement on Friday with the US Department of Justice and other government agencies over accusations that it shortchanged Medicaid...The move comes after a month of controversy over charges that Mylan improperly classified its EpiPen allergy device in reports to the Medicaid Drug Rebate Program. Under this program, companies must accurately report — and pay — a rebate on drugs paid for by the agency...Mylan, however, had been reporting EpiPen as a generic product for nearly a decade. And this is an important distinction, because classifications are used to determine the size of rebates that companies pay Medicaid. Rebates, which companies pay in exchange for having their products covered, are lower for generics — 13 percent versus 23 percent for a brand-name product.