- U.S. government suspends enrollment in Cigna Medicare Advantage, drug plans (reuters.com)
U.S. government has suspended new enrollment in Cigna Corp's Medicare Advantage health plans for seniors and standalone Medicare prescription drug plans, citing noncompliance in its appeals and grievances procedures...Officials also found problems with the administration of its covered drug plans and compliance program, such as not properly handling prior authorization and exception requests... Centers for Medicare and Medicaid said Cigna's deficiencies posed "a serious threat to the health and safety of Medicare beneficiaries" and followed years of noncompliance….Sanctions will remain in place until they are corrected and will likely not recur...Cigna plans to be bought by Anthem Inc in a $45 billion deal that is under review by antitrust regulators.
- CMS demands scrutiny of opioids, antipsychotics in Medicaid (modernhealthcare.com)2016 Updates to the Child and Adult Core Health Care Quality Measurement Sets (medicaid.gov)
CMS plans to more closely track the use of opioids by adults and antipsychotics among children and adolescents with new quality measures for Medicaid and the Children's Health Insurance Program...The agency issued a notice this month outlining the new measures, which come amid a national epidemic of opioid abuse and a rising unease with the high rates of antipsychotic medications prescribed to minors for off-label uses...CMS will require Medicaid programs...to track the use of opioids at high dosages acquired from four or more providers and pharmacies by beneficiaries who don't have cancer...The measure is intended to indicate inappropriate prescribing or fragmented care...American Pharmacists Association said the new Medicaid measure could help identify patterns of opioid misuse...The CHIP measure, meanwhile, would track the percentage of children and adolescents who are on two or more antipsychotic medications at the same time...an analysis by HHS' Office of Inspector General found that 92% of antipsychotics taken by Medicaid children in five states were prescribed for off-label uses...The use of multiple antipsychotic medications “is seldom justified and is an appropriate focus for a quality measure,”...children on Medicaid are prescribed antipsychotics at much higher rates than privately insured children.
- 5 things to know about CMS’ mandatory bundled payment program (healthcareitnews.com)
CMS announced the first mandatory test of shared-risk, outcomes-based payment model and the first initiative to make hospitals financially-responsible for patient recovery, 90-days after a knee or hip replacement surgery…The landmark program, Comprehensive Care for Joint Replacement, goes into effect April 1, 2016. Patient engagement and care coordination technology will be key to helping hospitals meet cost containment requirements…can lead to lower costs and increased healthcare quality…Healthcare institutions and leaders should know five items to move forward into the coordinated care initiative:
- 789 hospitals will be impacted
- 500,000 patients can participate, annually
- Quality matters. Hospitals must adhere to strict quality metrics and keep down care costs from admissions to 90 days after discharge
- Hospitals can donate $1,000 per Medicare beneficiary for patient engagement IT and services
- CMS will provide incentives for Patient Reported Outcomes
- Are providers in for a rude awakening about ICD-10? (revenuecycleinsights.com)ICD-10 problems persist for some healthcare providers (revenuecycleinsights.com)
It’s far too early to declare with certainty the impact of the ICD-10 transition on healthcare revenue cycles and productivity…Initial data shows the apocalyptic warnings about ICD-10 immediately leading to claims rejection chaos were misplaced. The Centers for Medicare and Medicaid Services late last month said invalid ICD-10 codes comprised only 0.09% of error-based denials from October 1 through October 27…While CMS said it was “pleased to report that claims are processing normally,” it’s worth keeping in mind that the government agency has taken several temporary steps to smooth the transition to ICD-10 which may be masking problems that could manifest themselves down the road, including a claims denial amnesty for 12 months and advance payments to physicians in the event of processing problems related to ICD-10… Providers that considered themselves unprepared for ICD-10 as October 1 approached shouldn’t assume their currently low claims rejection rates mean their self-assessment was overly pessimistic. If they felt they were unprepared, they probably were. And if they were unprepared for ICD-10 on October 1, they probably still are…To avoid an unpleasant reality check down the road, providers with any doubts about their ICD-10 readiness should continue training and testing.
- Providers slam CMS proposal meant to curb drug abuse (modernhealthcare.com)
Providers are urging the CMS to drop a proposal aimed at combating prescription drug abuse. They say mandating a review of state-run drug prescription databases could lead to inaccurate information and would be an administrative burden for them. They also say frequent prescription changes might reveal a lack of coordination among providers, not drug abuse...As part of a proposed rule on changes to discharge plans, the CMS suggested mandating that providers consult a patient's history on their respective state's prescription-drug monitoring program. The goal is to identify a patient's risk of nonmedical use of controlled substances by tracking substance-use disorders...“Requiring their use for all patients would overwhelm current systems and make it impossible for them to focus on the true at-risk groups they are intended to serve”...the required use of the PDMP for all patients will slow down the discharge process unnecessarily without adding value for patient care...Under the proposed rule, first announced in a November overhaul of the discharge process for hospitals, rehabilitation facilities and home health agencies, providers would be required to develop a discharge plan within 24 hours of a patient's admission or registration. They would have to complete that plan before the patient is discharged.
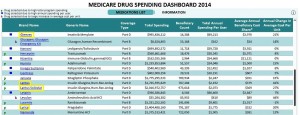
- Big Pharma’s steady double-digit price hikes cost Medicare billions (fiercepharma.com)Medicare drug costs rose sharply in 2014 (statnews.com)Medicare Drug Spending Dashboard 2014 (cms.gov)The CMS Blog: Medicare Drug Spending Dashboard (blog.cms.gov)
Sanofi, Pfizer, Novartis and peers ratchet up prices on blockbuster meds to reap big sales gains…a new report from the Center for Medicare and Medicaid Services puts some numbers to that claim. They won't resolve the debate over which price increases are "justified," but they do highlight some commonly used meds whose sales growth (grew)--and Medicare spending--depends more on rising prices than on rising demand.
- Vimovo...price hike at 543% for 2014... boost helped send spending on the drug up past $38 million from just over $7 million in 2013…patients using the drug only grew by 8%.
- Targretin...unit cost rose by 123% last year, to $145.65...CMS shelled out $73.5 million, more than double its 2013 spending…increase in patients of just 12%.
- CMS laid out $1.725 billion for Lantus last year, a $400 million increase year-over-year despite a 6% decline in patient count.
- CMS spent another $2.02 billion for Lantus Solostar, an increase of almost $700 million, or about 50% year-over-year...patient growth amounted to 13%.
- Gleevec sent CMS' unit costs up by 21% last year, to $179.93...that pushed spending per user to $69,212. The number of patients using the drug ticked upward by 5%...spending on the drug grew by 28%, to almost $1 billion.
- Lyrica...up in price...about 20%...to $4.28 per pill. Medicare spent $1.4 billion on the drug in 2014, up from just over $1 billion in 2013...patients grew by 7%.
When Sanofi, Pfizer and Novartis were raising their prices...they were fighting to fill patent-cliff sales gaps and scrambling to refill their pipelines of prospective new drugs. They were also spending billions on R&D--and on stock buybacks, dividends and other shareholder-friendly moves. Horizon and Valeant, by contrast, aren't big R&D spenders; Valeant, at least, has defended its price hikes as necessary to deliver returns to shareholders.
- Arizona inspectors find Theranos lab issues (azcentral.com)Safeway to dissolve partnership with Theranos (pharmacist.com)
Before…Theranos suspended use of its finger-prick blood draws in September because of Food and Drug Administration concerns, the company tangled with Arizona lab regulators over testing instruments and lab practices…Theranos, which operates retail locations inside 40 Walgreens stores across metro Phoenix, did not always meet lab regulations before taking corrective steps, according to inspection reports…After an April 2 survey of the company's Scottsdale lab, Arizona Department of Health Services inspectors noted four "deficiencies" at the lab...The state inspectors conducted the survey on behalf of the federal Centers for Medicare and Medicaid Services, which regulates laboratory testing…The four issues concerned proficiency testing, validation of instruments used to analyze blood samples, humidity levels outside of acceptable ranges for some lab instruments and how blood-sample collections were dated…In September, state lab inspectors said that Theranos did not meet proficiency testing standards for certain substances, including toxicology and four other regulated substances.
- Retail Pharmacist MTM Roles Supported by US House (pharmacytimes.com)
More than 40 members of the House of Representatives have expressed support for greater pharmacist roles in improvements made to Medicare Part D’s medication therapy management program...CMS announced plans to improve MTM with its Part D Enhanced MTM model in September 2015. The enhanced model aims to look at additional incentives and flexibilities to achieve the goals of the program...Some of those goals include increased communication with pharmacists, prescribers, and patients; improved patient knowledge; reduced medication problems; and improved compliance with medication protocols...The enhanced MTM model test will launch in January 2017...Some of the medication adherence concerns that the Congressional members noted were:
- Nonadherence costs the United States $290 billion annually and makes up 13% of total health care expenditures.
- Patients with several chronic conditions comprise two-thirds of all hospital admissions and are 100 times more likely to have a preventable admission.
- These patients with several chronic conditions visit many different physicians in a year and receive around 50 prescriptions annually on average.
- MTM is currently poorly integrated into health systems.
Congressional leaders called for retail pharmacists to be included in the enhanced MTM models that will be tested, citing how pharmacists have been shown to improve patient health, reduce costs through fewer hospitalizations and readmissions, and increase patient involvement in their own medication management...Our seniors deserve the most robust and effective MTM program possible—one that includes the utilization of the most trained and highly skilled providers medication management services: local retail community pharmacists...
- Inside the Impossibly Byzantine World of Prescription Drug Prices (realclearhealth.com)
Even for people whose job requires them to know this stuff, drug pricing is hopelessly complex. That helps explain why, for all the debate over drug costs these days, there’s surprisingly little detail about what anybody actually is paying for prescription medicines..."We have list prices, wholesale prices, average wholesale prices, rebates, supplemental rebates, mark-ups, outpatient vs. inpatient, formularies, patent expirations,"..."Most of that information is not available or well understood by the public."...This all raises the question: Just what the heck is the point of the list price anyway?...The short answer is that the list price is a drug company’s opening bid in negotiations with the insurance plans, government programs, and health care providers that purchase its medicines...The list price helps establish that initial starting point...In other words, the list price is not dissimilar from sticker prices on new cars...
- Amid Growing Rx Costs, No Consensus on Addressing Access (realclearhealth.com)
…stakeholders gathered at HHS' Pharmaceutical Forum…CMS Acting Administrator Andy Slavitt said millions of Medicare and Medicaid beneficiaries, as well as individuals enrolled in the Children's Health Insurance Program or health plans through the Affordable Care Act's insurance exchanges, "rely on prescription medications to manage chronic illnesses and treat acute conditions." However, surveys have shown "that as costs go up, so does everyone's anxiety about their continued access to their prescription medicine," he said…"As we encourage the development of new generations of highly targeted, personalized therapies, we need strategies for ensuring access to these innovations."
Laying Out the Problem
What's Been Proposed?
Negotiating Drug Prices, Increasing Rebates in Medicare
Cost-Sharing Caps
Expediting Drug Approval
Reforming Specialty Drug Reimbursements
No Consensus on Which Plan To Choose