- ICD-10 Could Challenge Emergency Rooms (pharmacytimes.com)
…changeover to ICD-10 medical diagnosis codes could complicate tasks in emergency departments…researchers...looked at more than 24,000 clinical encounters in the emergency room, they found that nearly a quarter could be assigned incorrect ICD-10 codes…also…27% of 1830 ICD-9 indicator codes commonly used by emergency physicians had convoluted mappings to ICD-10 codes that could pose problems for clinical documentation, reimbursement, disease reporting, and justifying hospital admissions…Depending on the analytic programs that the pharmacies use to predict how much medications to store and how complex the transition to ICD-10 is, pharmacies might have shortages of medications due to inaccurate reports and algorithms..
- 3 ways pharmacies can build CMS Star Ratings (drugtopics.modernmedicine.com)
Pharmacists can adapt to the evolution of their industry by understanding treatment guidelines, learning about local physician practices, and improving patient adherence,...these actions contribute to quality healthcare...This matters to pharmacists because they’re increasingly facing pressure to join preferred networks that link them to the success or failure of health plans… Medicare Star Ratings… help…patients choose which plan to enroll in… Plans with low Star Ratings…risk losing their CMS contract...
- Safety net hospitals say new rating system doesn’t consider socio-economic factors (modernhealthcare.com)Medicare.gov Hospital Compare (medicare.gov)
...new federal tool aimed at helping patients determine the best hospital for their care is raising questions over whether it provides an accurate assessment of quality.. CMS is developing a hospital quality star-rating system for the Hospital Compare website… We are not confident that the measures currently available…to create a single, methodologically sound rating of all aspects of hospital quality,".. should incorporate risk adjustment for socio-economic factors so results reflect differences in treatment across hospitals.
- Critical access hospitals losing money, but credit ratings safe over political support, Fitch says (healthcarefinancenews.com)
With revenue sliding, margins thinning and cash flow very light, these facilities lack reserves to offset market volatility…critical access hospitals will continue to earn less, Fitch Ratings this week said it does not expect the financial struggles to affect these hospitals' credit ratings due to their near 100 percent reimbursement from Medicare and political support that will stave off any attempt to cut payments...
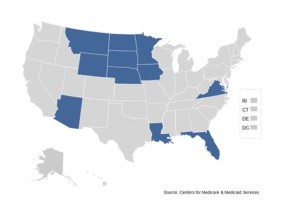
- CMS announces Part D Enhanced Medication Therapy Management Model (cms.gov)
Centers for Medicare & Medicaid Services Center for Medicare and Medicaid Innovation announced a model to test strategies to improve medication use...Medication therapy management,…can improve health care and outcomes for patients and has the potential to lower overall health care costs….Part D Enhanced Medication Therapy Management model will assess whether providing selected Medicare Prescription Drug Plans with additional incentives and flexibilities to design and implement innovative programs will better achieve the overall goals for MTM programs, including:
- improving compliance with medication protocols, including high-cost drugs, ensuring that beneficiaries get the medications they need, and they are used properly;
- reducing medication-related problems, such as duplicative or harmful prescription drugs, or suboptimal treatments;
- increasing patients’ knowledge of their medications to better achieve their or their prescribers’ goals of therapy;
- improving communication among prescribers, pharmacists, caregivers and patients.
Enhanced MTM model test will begin January 1, 2017 with a five-year performance period. CMS will test the model in 5 Part D regions....
- Inpatient Payment Rule for 2016 Continues Volume-to-Value Shift (ashp.org)
Medicare program's shift from volume to value continues with the finalization of the regulation setting inpatient payment rates for fiscal year 2016, the Centers for Medicare and Medicaid Services announced on July 31…annual update to Medicare's inpatient prospective payment system affects discharges occurring on or after October 1, 2015,..
- Hospital-acquired conditions reduction program…will continue its policy of reducing by 1% the reimbursement rate of hospitals in the bottom performance quartile...
- Value-based purchasing program…incentivizes rather than penalizes hospitals, will include new measures during 2016 that will be used for 2018 payment calculations, including one measure directly related to medication use.
- Add-on payments…authorizes a "new technology add-on payment" for blinatumomab,…for the treatment of a form of B-cell acute lymphoblastic leukemia…maximum add-on payment for the drug during 2016 is $27,017.85 per case,..authorize add-on payments for new technologies or medical services—including drugs—that produce greater clinical benefits than existing technologies..
- Update on "two-midnight rule."…rule was intended to clarify when patients should be treated as outpatients—generally under observation status—or admitted as inpatients…patients who are expected to require care spanning two midnights (i.e., 12:00 a.m. on two consecutive days) should be admitted as inpatients,… although inpatients and patients on observation status receive the same care, observation patients face higher out-of-pocket costs for medications because Medicare pays differently for drugs in inpatient and outpatient settings.
- Industry eyes calendar as ICD-10 countdown begins (healthcareitnews.com)
Less than six weeks from an oft-delayed deadline,..Questions abound regarding the financial repercussions of the coding format conversion across the provider spectrum, but especially for small hospitals and physician clinics…biggest fear is that a blizzard of claims denials… many providers are braced for a dramatic fall-off in revenues once the deadline hits…as high as 40 percent revenue loss in the first few weeks. Uncertainty reigns throughout the provider, payer and vendor sectors..
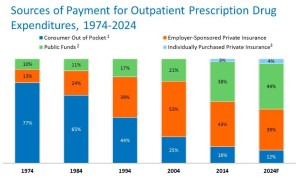
- Here s Who Will Pay For Prescription Drugs in 2024 (drugchannels.net)
Today, I (Adam J. Fein) identify new insights about payments in the 2024 drug market. As the charts below show:
- CMS expects the employer-sponsored insurance market to be slightly more resilient than it had previously projected.
- By 2018, however, Medicare, Medicaid, and other public programs will pay more than employers for drugs.
- CMS still projects that individually-purchased private insurance (via exchanges) will account for a small share of drug spending.
- CMS appoints ICD-10 ombudsman (healthcareitnews.com)
William Rogers, MD, director of the Physicians Regulatory Issues Team at the Centers for Medicare and Medicaid Services, will act as ICD-10 ombudsman to the federal agency, He will work out of an ICD-10 coordination center in Baltimore.. Implementation of ICD-10 is only 34 days away… CMS has said it will not deny claims as long as the right code family is used, the agency will not send back a message if the wrong code is used.
- Medicare Bundled Payment Gains Momentum With Hospitals, Nursing Homes (forbes.com)
...when medical care providers aren’t forced to accept bundled payments…that could cost them money if the care isn’t better and costs aren’t in check, they are willing to embrace such new reimbursement…about 9% of U.S. acute care hospitals and 7% of skilled nursing facilities are voluntarily assuming financial risk by participating in the latest phase of the… Bundled Payments for Care Improvement Initiative…This means these providers have agreed — long before it’s mandated — to take on financial risk that they can provide the necessary quality medical care for one bundled fee, grouping all of the services involved in an episode.